
I’m only sort of talking about cancer when I say that– more on that in a minute though.
See, when you start to reach a point in your journey where you start to feel like you’re breaking through plateaus, that’s when life starts to feel somewhat normal again. You can do the old things you used to do, sure, but they’re… different. Lately, I’m starting to feel less different in a lot of ways, and it feels good.
Now, that’s not to say I’m anywhere near an approximation of “old me” in many ways, but there are some notable changes:
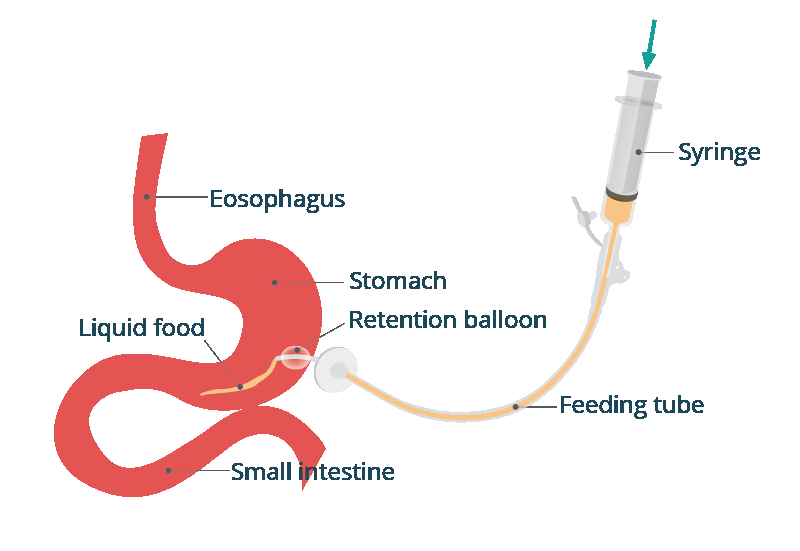
- The quality of volume of my saliva and mucus is starting to improve, and I don’t have to scrub the buildup off of my tongue daily.
- My taste is starting to claw back some flavors, or at least essences, even if it is easily the biggest lag of all my treatment side effects so far.
- My fatigue hasn’t improved much, but my ability to manage it has. I drink about double the caffeine that pre-cancer me used to, which is an increase of two cups of coffee per day to four or five, and about half the week I’m not waking up to pee three or four times per night.
- My short term memory recall is still ass, but I’m getting better about writing things in my Notes app or on a physical notebook.
- I’ve gained a whopping two pounds. Only fifteen more to go.
I’m averaging about one hockey game per week, and I am ruthlessly enforcing my limits out there. In beer league there can be a tendency for guys to stay “on shift” (out on the ice) too long, but I am the opposite. Rarely do I lose track of time; if I sense I’m close to two minutes into a shift I look for the first opportunity to climb back over the wall– less if I’ve had to defend a breakaway on that shift. I wish I could get back to being someone who could handle defending multiple rushes per shift, but it’s going to be a while before I’m that guy again.
I haven’t prioritized going into the woods since the opening weekend of elk archery but tomorrow I’m skipping out on being responsible for a day to try and find a bear in a unit I haven’t visited in a couple years to try my luck in the pouring rain. My intentions are pure– take it easy, be deliberate in all that I do, and do not take anything even resembling a risky decision. The weather will be against me and the Olympic rainforest is absolutely unforgiving in the fall; this is not the time to press my luck. If God decides I’ve been patient enough these last five years maybe my next entry will be written cloaked in a bear skin– or maybe my next entry will be titled, “how to activate your Garmin InReach SOS.” My guess is it will be something in between, given my luck. (Author’s note: This did not happen, I woke up after four hours of sleep, saw it was storming outside, and decided I was going to take a rest day.)
Speaking of taking risks, it’s time to expand more on the cliffhanger from last week: Sarah.
============
Hoo boy. What a journey. As of this writing it’s been over one calendar month since I decided to pull the trigger on telling Sarah how I felt. Despite the loss of confidence, my body image issues, my emotional baggage, and my extreme desire to not fuck up a good friendship… I decided to go for it.
The existential crisis that cancer presents you with is different than an acute one like a car accident, combat, or bad fall. Sure, you can walk away from those things with a new outlook on life, especially if they require a long recovery due to injury, or if there was some sort of psychological scarring– but cancer hit me differently than any of those things. I was a hostage in my own body to a very dangerous and unpredictable assailant, and just like is the case in many hostage rescues, the rescuers can do just as much damage as the hostiles.
I say all of that because when I decided to go for it after two weeks of deliberating, including a couple conversations with my psychologist and cognitive therapist, my calculation of what I decided an acceptable risk was had changed significantly from “old me.” Now the fear of the “what if” and “things left unsaid/undone” is a massively weighted factor in my decision making cycle. I could have five months left, five years, or fifty years– I don’t know. It’s not unlikely that God has fixed the time and place of my death so living like I’m trying to compete against that feels pointless.
As an Army officer we are conditioned to always plan off of the “most dangerous course of action” so that we are prepared to deal with the less severe “most likely course of action.” This trains your mind to only see the most devastating impacts of being wrong, and does not do much to reinforce a positive mindset that tells you what is at stake if you don’t take that big risk.
I went from feeling 2025 was going to be the undisputed champion of, “shittiest year of my life” to “wow, life comes at you fast.” The last couple years of being close friends made the transition to “couple” almost effortless and just about completely deleted the courtship phase of the relationship. Now, I still do take her on a date every week, and we are planning out future overnight travels, but we were so comfortable together already that the trust and respect was already pre-positioned– all we had to do was explore the romantic/intimate side of our new situation.
In a lot of ways, “new me” extends beyond what I physically bring to the table now. There’s also been a massive spiritual, emotional, and moral shift. I’m making big, bold, decisions that were somewhat uncharacteristic of old me. At work life, with my personal life, and with my romantic life. What I mean is, I’m trying to do this the “right way” for once. She has the advantage of knowing a ton about me already through osmosis and general conversation when we were “just friends” but I committed to being vulnerable right off the bat with her and becoming completely transparent. The good, the bad, the ugly– I disclosed everything over the first week of our new relationship. Get it all out there now, fuck it, nobody can say later I was holding anything back and coming at this without the purest of intentions.
The flip side to this is that instead of slowly releasing the codes to the bombs, I just dumped them all into her lap. She possesses every key now. But that’s what love is, right? Giving someone the means to destroy you and trusting them not to?
This blog isn’t primarily focused on relationships, but that is part of the journey. This is part of the journey. She is part of the journey now. She’s expressed a deep regret over not “being there more for you” when I was sick, but she’s also not the first person to say that… and that’s ok. Everyone has their own lives, their own crisis to manage, their own priorities. There’s a very short list of people I’m disappointed in for not showing up for me more, and she’s not on it.
============
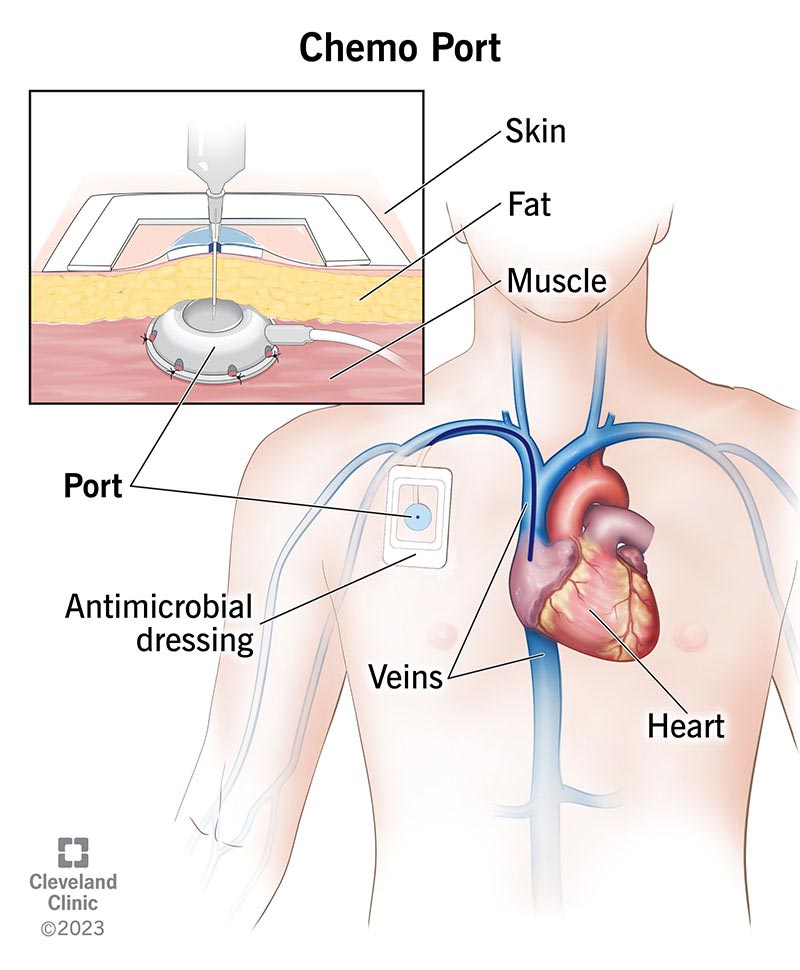
There have been a slew of medical occurrences since I last posted an entry. Three times per week I’m receiving physical rehab (strength training and conditioning), once weekly I see a cognitive therapist, once every 3-4 weeks I see an outpatient psychologist, and most recently I did my check-in with the ENT. ENT, per tradition, scoped me and gave me an ultrasound. Three times each, to be precise. Once was the resident, once the resident and the chief, and once just the chief.
You might remember LTC Sierra, chief of ENT at the Army hospital, from earlier in our tale. She’s still there, and as usual she was in to see me after the resident was done with his initial run. Long story short, she thinks I’m fine but wanted to possibly biopsy me again because she doesn’t like the look of the lymph node that was treated when the cancer metastasized. She told me she’d deliberate on it, consult some colleagues, and get back to me. Great. Grand. Wonderful. NO MORE CANCER ON THE BUS.
That friday she ended up calling me back and told me that she ruled out a biopsy, but wanted to get in touch with Dr Panner (RadOnc) at the cancer center to see if they could order some sort of fancy new blood test to see if it was, you know, cancer again. I haven’t heard back on this in a couple weeks, but I have another PET in a couple weeks, so inshallah, I guess.
The views and opinions presented herein are those of the author and do not necessarily represent the views of the Department of Defense or the U.S. Army.





You must be logged in to post a comment.